Drone warfare is stretching medevac timelines to days. See how AI-ready, connected field hospitals can deliver prolonged care and save lives in contested zones.
High-intensity conflict has quietly broken one of the U.S. military’s most relied-on assumptions: that casualties can be moved quickly to higher levels of care.
In Ukraine, evacuations that “should take minutes” are reportedly stretching to 72–96 hours. Drones hunt ambulances. Helicopters can’t count on air superiority. Medical teams are forced to treat longer, closer to the fight, and under constant surveillance.
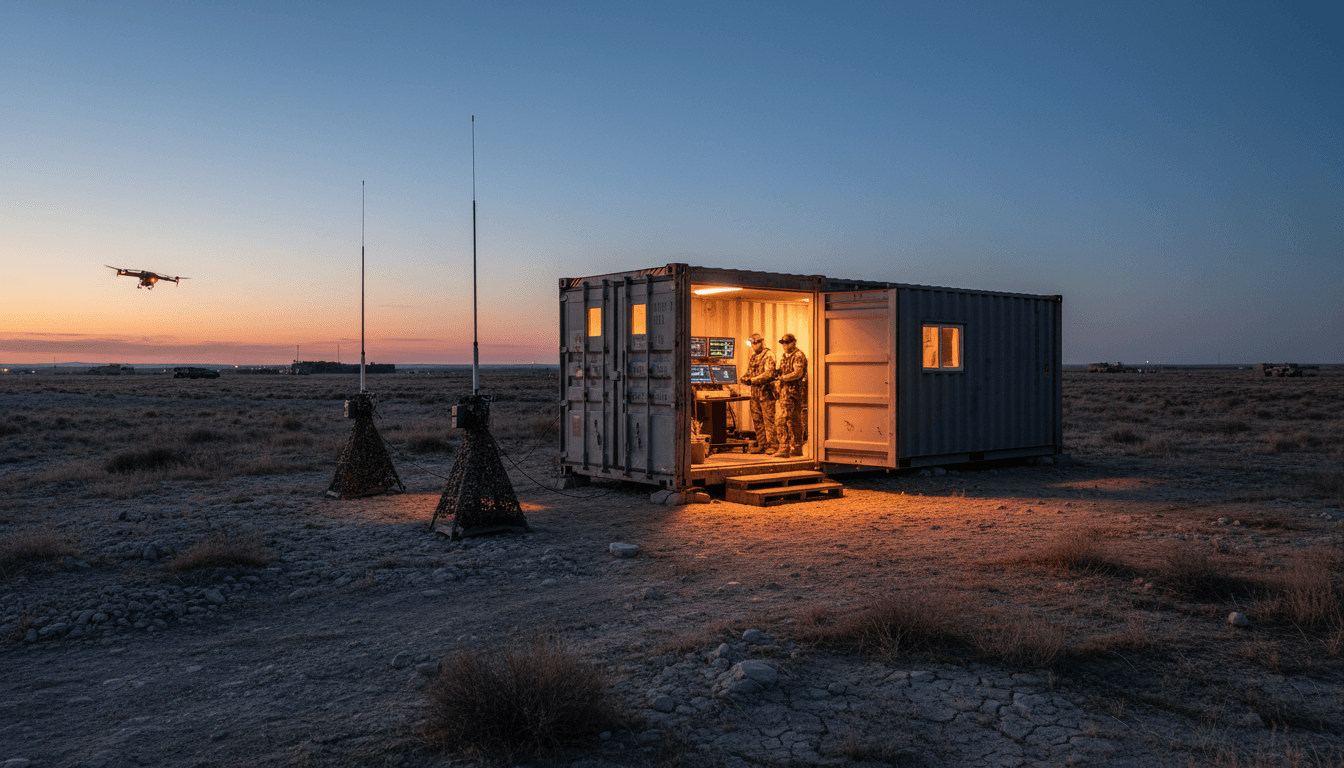
That’s the context for a new class of defense innovation: connected, hardened, low-signature “field hospitals in a box.” A startup called Valinor is building one called Harbor—a 20-foot container that arrives as physical infrastructure and as a software platform for remote monitoring, telehealth, and device control. It’s a concrete example of what this “AI in Defense & National Security” series keeps returning to: AI isn’t just about targeting and sensors—it’s also about sustaining humans when the battlefield stops being permissive.
Why battlefield medicine is changing faster than doctrine
Modern battlefield medicine is being reshaped by a simple, harsh shift: casualty evacuation is no longer guaranteed. When medevac timelines stretch from minutes into days, the whole medical system has to re-balance.
The “golden hour” is harder to buy with airlift
For the last two decades, U.S. forces often operated with strong air dominance and mature logistics. That enabled quick evacuation and layered care.
The drone era flips the risk calculus:
- Airspace is contested even when neither side has classic air superiority.
- Forward movement is observable (persistent ISR, inexpensive drones, quick strike cycles).
- Medical facilities and routes are targetable—not just by chance, but deliberately.
When evacuation slows down, the field medical problem changes from “stabilize and move” to “stabilize, monitor, treat, and hold.” That requires infrastructure that looks less like a tent and more like a defensible node in a network.
Prolonged casualty care becomes a systems problem
Prolonged casualty care isn’t only about clinical skill. It’s also about:
- Power stability
- Communications resilience
- Supply tracking
- Patient monitoring at scale
- Documentation and continuity of care
Once you’re treating multiple casualties over days, you need a systems approach—and that’s exactly where software, networking, and AI-assisted workflows start paying for themselves.
The “field hospital in a box” model: faster setup, harder to kill
The Harbor concept is direct: put battlefield medical capability into a 20-foot shipping container that can be configured for different missions—damage control, stabilization, or prolonged casualty care.
The key idea isn’t the container itself. The key idea is standardizing a modular, manufacturable unit that can be deployed quickly, protected better than tents, and upgraded like a platform.
Here are the details that matter for planners and acquisition teams:
- Setup time: described as “minutes,” not days
- Starting price: around $300,000 per unit
- Manufacturing claim: capacity to produce 300 units in 2026 if contracted
By comparison, academic data cited in the source article notes that an Army field hospital can take about 72 hours to set up (per 2018 studies), and a 2015 study of Afghanistan deployments put operating costs at over $3 million per month.
Those numbers aren’t apples-to-apples (a container clinic isn’t a full hospital). But they expose a procurement reality: when casualties surge and evacuation slows, you need scalable “middle layer” care—fast.
Hardened and defensible changes the survivability equation
Tents are fast, but they’re fragile. A hardened exterior changes decisions commanders can make:
- Where the unit can be placed
- How long it can remain in place
- How much security it requires
If the exterior can be hardened against ballistics and supports integration with counter-drone defenses, it becomes more than a medical tent replacement—it becomes a node designed to survive contact.
Connected care under fire: where AI actually fits
A lot of defense AI conversations drift toward autonomy and targeting. Battlefield medicine is a better test of maturity: if your AI and networks can’t handle a chaotic, contested environment with real consequences, they’re not ready.
The Harbor approach is essentially “digitize the care environment,” then use connectivity to extend expertise forward.
Telehealth + mesh networks: expertise doesn’t have to be co-located
Valinor’s partner Anduril is described as enabling telehealth over a mesh network while managing electromagnetic signatures.
That combination matters because bandwidth and detectability are linked:
- The more you transmit, the more you risk detection.
- The more you reduce signature, the more you constrain data flow.
A smart architecture aims to do both:
- Prioritize critical patient telemetry
- Cache and sync non-urgent data
- Support offline clinical content
- Use burst transmissions and routing discipline
This is where “AI-ready networks” stop being a buzz phrase and become a survival requirement.
Remote monitoring: triage becomes data-driven, not vibes-driven
Integrated sensors and monitoring can improve emergency triage outcomes, and the logic is straightforward: humans miss things under stress; sensors don’t get tired.
In practical terms, a connected container can support:
- Continuous vitals trending (not just spot checks)
- Automated alerts for deterioration
- Standardized handoffs and documentation
AI doesn’t need to “diagnose” to be useful. A more realistic near-term win is clinical decision support:
- Highlight abnormal trends early
- Recommend checklists or protocols
- Flag drug-device interactions
- Suggest evacuation priority based on risk scores
That’s AI doing what it’s good at: pattern recognition, prioritization, and consistency.
Remote device control is powerful—and needs guardrails
The source article notes the ability to remotely control devices like ventilators and IV pumps.
That’s a big deal. It can:
- Extend scarce expertise to austere sites
- Reduce workload for overwhelmed medics
- Enable standardized therapy protocols across multiple sites
It also introduces new risk:
- Cybersecurity (device and network)
- Authentication and authorization
- Fail-safe operation when comms drop
My stance: remote control should be designed as “assist-first,” not “control-first.” In other words, prioritize remote configuration, verification, and coaching over continuous remote steering—unless you have hardened comms, strong identity, and clearly defined clinical authority.
What procurement teams should ask before buying “connected medicine”
If you’re evaluating containerized or connected medical systems for defense or national security, the differentiator won’t be the demo. It’ll be the answers to a few uncomfortable questions.
1) How does it operate when disconnected?
The battlefield is intermittent by default. A serious system needs:
- Local-first patient records and monitoring
- Offline clinical references (video guides, protocols)
- Store-and-forward syncing
If it’s cloud-dependent, it’s a non-starter for contested environments.
2) What’s the electromagnetic signature management plan?
“Connected” is easy. Connected and low-signature is hard.
Ask how the system:
- Prioritizes data types
- Controls transmission power and timing
- Handles routing and relays
- Works under jamming conditions
3) How is cybersecurity handled for medical IoT and device control?
Medical devices are increasingly networked computers. Treat them like it.
Minimum expectations:
- Strong identity (device and user)
- Role-based access (clinical authority matters)
- Audit logs (who changed what, when)
- Secure updates (signed firmware/software)
4) What’s the sustainment model?
Containerized systems can look inexpensive upfront and become expensive later.
Procurement should demand clarity on:
- Spares and repair pathways
- Calibration schedules for sensors
- Battery and power subsystem replacement cycles
- Software update cadence and support
5) How quickly can clinicians be trained to use it under stress?
The best interface is the one a medic can operate at 3 a.m. while exhausted.
Look for:
- Short training pipelines
- Embedded checklists and guided workflows
- Simple modes for mass casualty events
A realistic vision: medical nodes as part of the battlefield network
Here’s the bigger connection to the “AI in Defense & National Security” series: the modern battlefield is a network of nodes—sensors, shooters, decision-makers, and sustainment. Medical care is one of those nodes.
Treating a medical unit as a node means it can:
- Share casualty status to support operational planning
- Improve evacuation prioritization when lift is scarce
- Reduce preventable deaths via earlier deterioration detection
- Enable remote specialists to extend capability forward
It also means medical infrastructure must be designed with the same seriousness as other nodes:
- Communications resilience
- Cybersecurity
- Signature management
- Rapid deployment and modular scaling
Harbor is notable because it’s built around that premise from the start: a physical treatment space that’s also an information system.
What leaders can do in 2026 planning cycles
As budgets tighten and modernization priorities compete, battlefield medicine can get framed as “support.” That’s the wrong mental model.
If evacuation is contested, medicine becomes operational. It shapes tempo, morale, and force preservation.
Three practical steps that fit near-term planning:
- Run a contested-medevac exercise that forces 48–96 hour holds and measures outcomes (clinical and operational).
- Pilot containerized care as a networked capability, not as stand-alone equipment—test comms, cyber, and signature constraints.
- Define an AI/analytics baseline for triage and monitoring (alerts, trending, documentation automation) before attempting advanced autonomy.
The next few years will reward programs that can scale quickly, survive in place, and keep clinicians connected without making them detectable.
Battlefield medicine for the drone era isn’t a niche problem. It’s a preview of how national security systems have to evolve: distributed, resilient, and intelligently connected—because the battlefield isn’t giving anyone time to build a perfect hospital anymore.