AI in insurance call centers won’t erase jobs—it will erase busywork. See where AI fits, what to automate safely, and how to improve CX and compliance.
AI in Insurance Call Centers: Jobs Won’t Vanish
A typical insurance contact center agent handles 40–60 calls per day. That’s not “customer service” in the cozy sense. It’s a production environment—measured in seconds, staffed for peaks, and judged on outcomes like first-call resolution, compliance adherence, and customer sentiment.
Now add December realities: claim spikes after winter storms, end‑of‑year policy changes, billing questions, and customers trying to squeeze in coverage adjustments before renewals. The phones don’t just ring—they pile up. When people ask, “Will AI replace call center jobs in insurance?” they’re reacting to that pressure and to the wave of AI voice assistants that sound confident but still miss the point.
Here’s my stance: AI won’t eliminate insurance call centers. It will eliminate a chunk of the work inside them. That’s good news—if you design it right. In the AI in Customer Service & Contact Centers series, this post focuses on what’s actually changing, why regulated insurance environments are different, and how to implement call center AI without torching customer trust.
Will AI replace insurance call center jobs? The real answer
AI will replace tasks, not the entire role. Insurance customer service is a mix of repeatable questions (great for automation) and emotionally loaded, high-stakes interactions (still best handled by people).
The work AI can reliably take on today includes:
- Identity checks and intent capture (routing the call correctly)
- Pulling policy details, coverage limits, billing status, claim status
- Drafting call notes and summaries
- Suggesting compliant phrasing and required disclosures
- Creating follow-up tasks, filling forms, updating CRM fields
But the role an agent plays—de‑escalation, judgment, empathy, exception-handling, and accountability—doesn’t disappear. It becomes more visible.
A useful way to think about it:
If a customer’s situation can be solved with a lookup and a script, AI should handle most of the lookup. If it requires judgment, a human should own the decision.
That human ownership matters even more in insurance because a “simple” call often isn’t simple. A billing question can turn into a coverage review. A claims status call can turn into a complaint. A policy change can raise underwriting questions.
Why insurance contact centers don’t automate like retail
Insurance call centers operate under a higher compliance burden than most industries. That changes what “good automation” looks like.
Compliance isn’t a checklist—it’s a live constraint
In insurance, agents have to follow rules about:
- What can and can’t be promised on coverage and claims outcomes
- Required disclosures and recorded consent
- Data privacy, authentication, and access control
- Documentation standards (who said what, when, and why)
If your AI assistant improvises—or even paraphrases too creatively—you don’t just get a bad customer experience. You risk misrepresentation.
That’s why the most effective call center AI systems in insurance are grounded in approved knowledge (policy language, product docs, process playbooks) and are designed to cite internal sources to the agent rather than “wing it” to the customer.
Product complexity is growing, and customers expect personalization
Personalization isn’t optional anymore. Research often cited in customer experience circles shows that 71% of customers expect personalized interactions, and 76% get frustrated when they don’t receive them. In insurance, that means callers expect the agent to understand their context quickly: prior claims, policy structure, endorsements, household members, payment history, prior interactions.
The challenge is obvious: humans can’t scan six systems in 30 seconds.
AI can.
When AI does the scanning and summarizing, agents can spend their limited time doing what customers actually value—explaining options and helping them choose.
What “good” AI in insurance customer service actually does
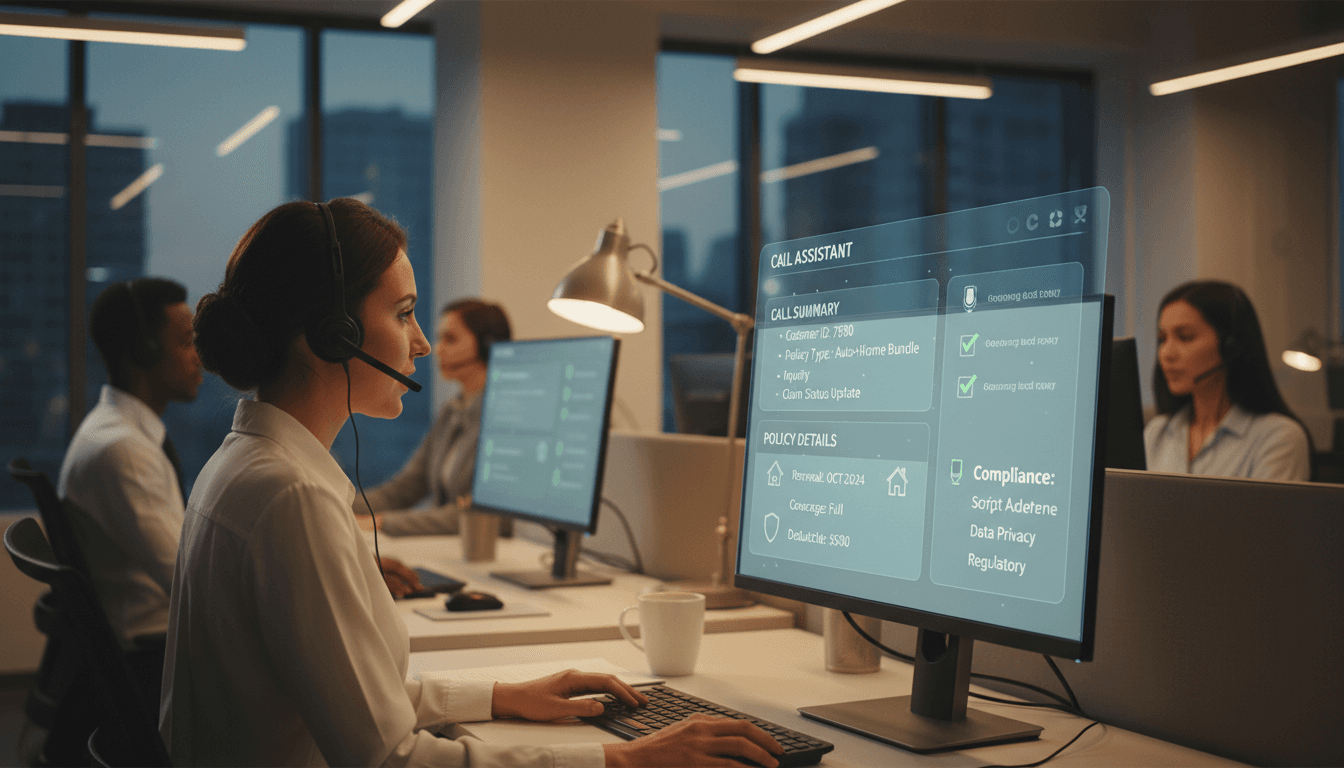
The best AI in insurance call centers behaves like a real-time copilot. It doesn’t replace the agent; it reduces the agent’s cognitive load.
1) Real-time answers that respect policy language
Agents need fast, precise answers under pressure. A well-designed AI assistant can:
- Retrieve the right snippet from internal knowledge
- Surface eligibility rules and exceptions
- Provide step-by-step process guidance
- Suggest compliant phrasing for tricky topics
This matters because speed without accuracy is dangerous in insurance. Your goal isn’t shorter calls at any cost. Your goal is fewer avoidable follow-ups and fewer compliance issues.
2) Next-best-action guidance (without turning agents into robots)
“Next best action” works when it’s helpful, not pushy.
In practice, this means the AI can recommend:
- The correct workflow based on call intent (billing, claims, policy service)
- A retention step when churn signals appear (fee waiver policy, payment plan options)
- A coverage review prompt when the customer’s life event suggests a gap
The agent still decides. AI suggests.
3) Automation of repetitive after-call work
After-call work is where time goes to die: documentation, ticket creation, wrap codes, follow-ups, emails, CRM updates.
AI can automate a large portion of this safely by:
- Generating structured call summaries
- Pre-filling fields based on the conversation
- Creating follow-up tasks with deadlines and owners
- Tagging interactions for analytics and quality review
This isn’t glamorous, but it’s where you’ll often see the cleanest ROI.
4) Quality, coaching, and consistency at scale
In peak season (hello, December), insurance contact centers often rely on temporary staffing, overtime, or outsourcing. That’s when consistency breaks.
AI-assisted coaching can help by:
- Flagging missing disclosures in real time
- Nudging agents toward correct workflows
- Highlighting policy constraints before the agent says something risky
This is also where AI helps BPO environments: faster ramp-up, less reliance on tribal knowledge, and fewer “agent roulette” outcomes.
The ROI isn’t “fewer agents.” It’s fewer friction points.
Cost reduction is part of the story, but it’s not the winning story.
From the source content, teams using AI in this context report results like:
- 30% increase in cross-selling and upselling opportunities
- 15% improvement in customer service productivity
- 20% growth in Net Promoter Score (NPS)
Those are big swings because they attack the real enemy: friction.
Here’s what friction looks like in insurance customer service:
- Customers waiting too long to reach a capable person (one commonly cited stat: 75% feel it takes too long to reach a representative)
- Agents searching multiple tools mid-call
- Inconsistent answers between agents or sites
- Rework from poor notes and missing documentation
- Transfers caused by misrouting or unclear intent
AI removes friction by compressing time-to-understanding. That’s the unit that matters.
A practical adoption plan for AI in contact centers (insurance edition)
If your goal is leads and measurable outcomes, you need a plan that’s operational, not theoretical.
Step 1: Pick 2–3 call types that are common and low-risk
Start where automation has the best chance of success:
- Billing and payment questions
- Proof of insurance / documentation requests
- Simple policy changes with clear rules (address update, vehicle change intake)
Avoid launching first on highly disputed claims or complex liability conversations.
Step 2: Define guardrails before you define features
In insurance, guardrails are the product.
Set rules for:
- Approved knowledge sources (and what’s out of scope)
- Confidence thresholds (when to escalate to a human)
- Required disclosures and compliance prompts
- Data handling (PII redaction, retention, role-based access)
A strong principle:
If the AI can’t cite where an answer came from internally, it shouldn’t present it as an answer.
Step 3: Measure the right KPIs (not just AHT)
Average Handle Time (AHT) matters, but it’s easy to game and dangerous to over-optimize.
Track a balanced set:
- First Call Resolution (FCR)
- Repeat contact rate within 7 days
- Transfer rate
- After-call work time
- QA/compliance score trends
- Customer sentiment and complaint rate
If AI lowers AHT but increases repeat contacts, you’ve created faster failure.
Step 4: Design for agent trust, not agent surveillance
Agents won’t adopt tools they don’t trust.
Make the AI:
- Transparent (show why it suggested something)
- Correctable (easy to edit summaries and notes)
- Non-punitive (coaching signals shouldn’t feel like “gotcha”)
The fastest way to kill adoption is to roll out AI as a monitoring tool first.
Step 5: Expand from customer service into the rest of the insurance value chain
This is where the broader AI in Insurance narrative gets interesting.
Once your contact center has reliable knowledge retrieval and workflow automation, it becomes a front door to:
- Claims triage and smart intake
- Fraud detection signals (pattern detection across interactions)
- Underwriting referrals (flagging risk changes)
- Proactive retention (predicting churn from interaction history)
The contact center is often the best place to start AI adoption because the feedback loop is immediate. You hear what works and what fails in real time.
People also ask: what happens to agents when AI arrives?
Agents become higher-skill roles. Not every agent wants that—and leaders should be honest about it—but it’s where the job is heading.
Expect shifts toward:
- Complex case ownership (fewer transfers, more resolution)
- Advisory conversations (coverage guidance, life-event changes)
- Empathy-heavy calls (catastrophe response, claim disputes)
- Fraud-aware listening (inconsistencies, escalation triggers)
- QA collaboration (helping refine knowledge and workflows)
This is the human-AI partnership that actually improves insurance customer experience.
What to do next if you’re evaluating call center AI
If you’re responsible for insurance customer service, operations, or digital transformation, don’t start with “Which chatbot should we buy?” Start with “Where do we lose time and trust?” Then map AI to those moments.
A simple next step: run a 2-week analysis of transcripts and call reasons, identify your top three friction points, and decide which ones can be reduced through (1) real-time agent assist, (2) workflow automation, or (3) better knowledge access.
This series focuses on practical AI in customer service and contact centers—because that’s where AI either earns trust fast or loses it permanently. Will AI replace insurance call center jobs? No. But it will replace the parts of the job that burn people out—and that’s exactly why you should take it seriously.