Record flu admissions and looming strikes are stress-testing NHS capacity. See what’s working, what isn’t, and what reform priorities matter now.
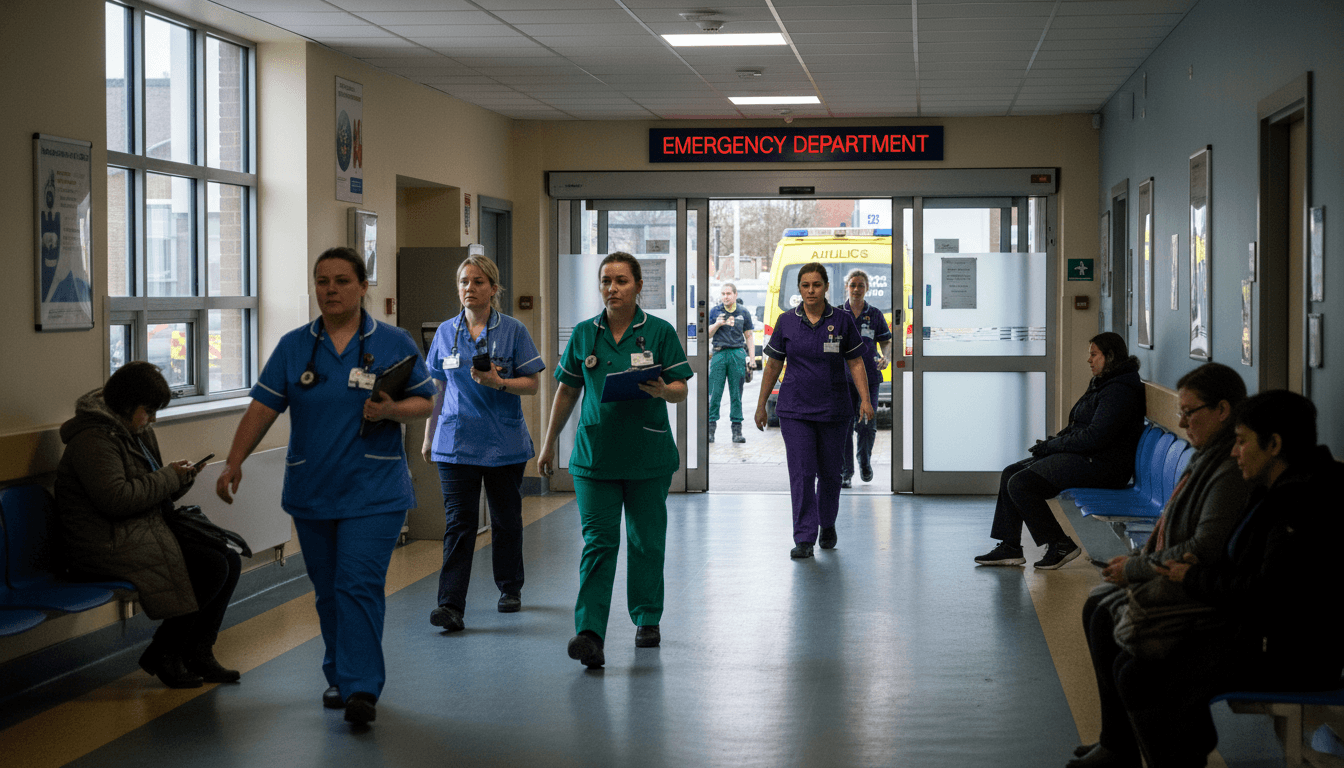
NHS Winter Pressure: Flu Surge, Strikes, and Reform
An average of 1,717 people a day were in hospital beds with flu last week in England. That’s not a typo—and it’s the highest on record for this time of year, with “no peak in sight yet.” Add the prospect of resident doctor industrial action in the run-up to Christmas and you get the kind of stress test that exposes what the NHS is doing well, and where the system still has brittle points.
This post sits within our Healthcare & NHS Reform series for a reason. Winter pressure isn’t just a seasonal headache; it’s a live case study in NHS capacity planning, urgent and emergency care flow, and what real healthcare reform has to prioritise if we want shorter waits and a more sustainable service.
The headline story is grim. The more useful story is practical: which parts of the system are holding up, which aren’t, and what we can do—now and long-term—to stop flu from swallowing elective capacity every winter.
What the winter data is really telling us
The key point: England’s urgent and emergency care system is already running hot, and flu is pushing it from “stretched” into “unstable.” The numbers give a clear early warning.
Last week’s reported pressures included:
- 1,717 flu patients per day in hospital (record for this point in winter)
- 10× higher than the comparable week in 2023 (160)
- 50%+ higher than the same week last year (1,098)
- 99,000 ambulance handovers at hospitals (about 4,500 more than last year)
- Ambulance handover times ~10 minutes faster than last year (a real operational improvement)
- NHS 111 received 11,338 more calls than the same week last year
Here’s why that mix matters. Flu doesn’t only add patients; it changes the shape of demand:
- It increases respiratory admissions that often require oxygen, monitoring, and longer stays.
- It pushes frail patients into decompensation (falls, delirium, dehydration), adding complexity.
- It clogs bed availability, which backs up emergency departments and slows ambulance offload.
If you want a single quotable sentence: Winter flu pressure isn’t an A&E problem—it’s a whole-hospital capacity problem.
The “double whammy”: why strikes amplify winter risk
The key point: industrial action during peak winter doesn’t just reduce workforce capacity; it disrupts the system’s ability to maintain flow. That’s a different kind of risk than “fewer staff on shift.”
When resident doctors strike, services typically prioritise emergencies and urgent care. The knock-on effects often land elsewhere:
Elective disruption creates a backlog that lasts months
Cancelled outpatient clinics and planned procedures don’t disappear. They rebook. That matters because winter flu already forces hospitals to flex beds into acute use.
A blunt reality I’ve seen in operational planning conversations: when flu admissions rise, elective work becomes the “shock absorber.” It’s the first thing to move because emergencies can’t be turned away.
If strikes hit at the same moment, the shock absorber fails—and you get:
- more cancellations
- longer waits for diagnostics and treatment
- slower discharge planning because teams are reallocated
Patient anxiety and demand shift
When people think “services are disrupted,” they don’t calmly wait for the best channel. They often:
- go straight to A&E “just in case”
- call 111 in higher volumes
- delay seeking help until symptoms worsen
That last point is the quiet killer of capacity. Late presentation means higher acuity, longer stays, and more pressure on beds.
The reform angle: a strike-prone workforce is a system design problem
I’m going to take a stance: repeated winter strikes are a sign we’ve built a workforce model that’s too fragile and too adversarial. Pay disputes are real. Training pressures are real. But if the system can be tipped into crisis by predictable disputes at predictable times, that’s a governance and resilience problem—not just an HR problem.
Long-term NHS reform has to include:
- clearer multi-year workforce settlements (less annual brinkmanship)
- better roster flexibility and cross-cover planning
- protected elective capacity that doesn’t collapse every winter
Vaccination is capacity planning (not just public health)
The key point: every prevented flu admission protects beds for cancer care, diagnostics, and planned surgery. Flu vaccination is a waiting list intervention.
The NHS has delivered almost 17 million flu jabs (16,905,349) so far—350,000 more than this time last year. That’s not a nice-to-have. That’s one of the few levers that reduces demand upstream without rationing care.
How flu jabs connect to waiting lists
When flu fills beds, hospitals cancel elective work because:
- post-op patients need step-down beds that aren’t available
- staffing gets redeployed to acute wards
- infection prevention rules reduce ward flexibility
So the connection is direct:
Reducing flu admissions is one of the fastest ways to protect elective throughput in winter.
Who benefits most (and why it matters for reform)
Targeted vaccination doesn’t just reduce overall cases; it reduces the most system-expensive cases:
- older adults with higher admission rates and longer stays
- people with COPD/asthma/heart disease at higher risk of complications
- carers and household contacts who can break transmission chains
From a sustainability standpoint, prevention that reduces high-cost admissions is exactly where the NHS gets the best return on effort.
Practical actions organisations can take now
If you work in an NHS-adjacent organisation, employer health, care home group, or local system partner, these are high-impact moves during late December:
- Run last-chance vaccination sessions with extended hours (after-work slots outperform “office hours” clinics).
- Use plain-language scripts for frontline teams (people respond to clarity: “Flu admissions are already at record levels; your jab helps keep you out of hospital.”)
- Target high-contact roles (care staff, community teams, patient-facing admin) to reduce transmission.
What’s working: signs of modernisation under pressure
The key point: some parts of the system are improving, and the improvements are measurable—especially in access channels and ambulance flow.
Despite higher demand, ambulance handover times were reported as almost 10 minutes faster than last year. That sounds small until you translate it into operations:
- 10 minutes multiplied across thousands of handovers is a lot of crew time returned to the road
- faster turnaround supports response times for the next call
- reduced queueing outside hospitals lowers clinical risk
111, online GP requests, and pharmacies aren’t “alternatives”—they’re load balancing
The NHS message to use 111 (phone or online) for non-life-threatening needs is more than a comms line. It’s load management.
Two details from the winter picture show how the model is changing:
- 98.7% of GP practices offer online consultation requests
- 8 million people used them in October
And community pharmacy support for common conditions (including access to some prescription-only treatments) is a genuinely useful shift when demand spikes.
Here’s the stance: When people can resolve sore throats, sinusitis, and earache quickly through pharmacy pathways, A&E becomes less crowded and GP capacity frees up for complex care. That’s what modernised access should do.
Urgent treatment centres and the “middle layer” problem
Opening more urgent treatment centres is the right direction, but only if the public can navigate the choices without confusion.
What tends to work in practice:
- 111 booking into urgent treatment slots (rather than walk-in uncertainty)
- clear local messaging on “what this site treats”
- integrated records so patients don’t repeat their story five times
This is where NHS reform becomes real: integration beats expansion. More sites help, but better routing and shared information helps more.
A resilience playbook for the rest of winter
The key point: the NHS needs short-term surge tactics and long-term capacity reform—and the winter data tells us exactly where to focus.
Short-term: protect flow, not just staffing
If your goal is safer urgent and emergency care, you protect flow:
- Discharge coordination: daily senior review, early transport planning, pharmacy prioritisation for discharge meds.
- Bed management discipline: ring-fence escalation beds with clear criteria, avoid “permanent escalation” becoming the norm.
- Respiratory pathways: rapid access clinics, home oximetry where appropriate, and clear safety-netting.
Medium-term: make prevention a winter capacity line item
Flu vaccination should sit in the same leadership dashboard as:
- bed occupancy
- ambulance handover delays
- A&E waits
- elective cancellations
If prevention isn’t measured like capacity, it won’t be resourced like capacity.
Long-term: reform priorities that winter keeps proving
Winter pressures reliably highlight the same structural needs:
- More resilient workforce planning (fewer crisis rotas, better retention, less churn)
- Better out-of-hospital capacity (community nursing, step-down beds, social care integration)
- Digitally-enabled access that’s consistent (not a postcode lottery of pathways)
- Protected elective capacity so waiting list recovery doesn’t collapse every December
A memorable one-liner that’s also true: If the NHS only “copes” in winter by cancelling planned care, it isn’t coping—it’s borrowing pain from the future.
Where this leaves patients—and what leaders should do next
Record flu admissions and the threat of strikes are a stress test the NHS didn’t ask for, but it’s one it has to pass. The encouraging bit is that some of the hard operational work is showing up in the data: faster ambulance handovers, higher uptake of online consultations, and expanded pharmacy pathways.
The less encouraging bit is familiar: when demand surges, the system still leans heavily on postponing elective care. That’s why NHS reform can’t just be about more funding or louder winter plans. It has to be about sustainable capacity, better workforce settlement models, and prevention that’s treated as core infrastructure.
If you’re working on healthcare strategy—whether inside the NHS, in a supplier organisation, or in local system partnerships—now’s the moment to ask a sharper question than “How do we get through winter?”
How do we stop winter from resetting the waiting list clock every year?