Remote robotic stroke treatment can cut hours off care for rural patients. See how AI-assisted telerobotics is making thrombectomy access realistic in 2026.
Remote Robotic Stroke Treatment: Faster Care Anywhere
A large-vessel stroke can destroy about 2 million neurons per minute while blood flow is blocked. That’s not a metaphor—it’s a clock with consequences. In an urban stroke center, an endovascular specialist can often begin an endovascular thrombectomy quickly. In remote regions, the same patient may spend six hours or more waiting for an aeromedical transfer before an expert even touches a catheter.
Most companies get this wrong: they treat access as a logistics problem alone. It’s also a capability distribution problem. If the expertise only exists in a handful of hospitals, you’ll always be fighting geography.
Remote robotics changes the shape of that fight. Instead of moving the patient to the surgeon, you move the surgeon’s hands—via a robotic system—closer to the patient. The reality? This is no longer a sci‑fi pitch. Recent demonstrations—from crosstown remote brain angiograms in Toronto to a transatlantic simulated thrombectomy between Florida and Scotland—show that telerobotic neurointerventions are shifting from “possible” to “plannable.” And for healthcare leaders watching AI and robotics transform industry after industry, this is one of the clearest, highest-stakes use cases yet.
Why remote robotic stroke treatment matters (and why now)
Remote robotic stroke treatment matters because EVT outcomes are time-dependent, and today’s stroke systems of care routinely leave rural and remote patients behind.
Endovascular thrombectomy (EVT) is the standard of care for many strokes caused by large clots blocking major brain arteries. A specialist navigates catheters and guidewires through the vascular system—often entering via the femoral artery in the groin—using X‑ray imaging guidance. It’s delicate, high-skill work that’s hard to staff everywhere.
Rural access isn’t a niche issue
The access gap shows up in Australia’s north (for example, patients in and around Darwin may require long transfers), but the same pattern exists in parts of the U.S., Canada, the EU, and across large geographies in Asia, Africa, and South America.
When a region lacks on-site neurointerventional coverage, the “solution” is often:
- Stabilize locally
- Arrange transport
- Hope the window for benefit hasn’t closed
That’s not good enough for a condition where minutes shape disability, long-term care cost, and quality of life.
The late-2025 inflection point
What’s different heading into 2026 is that the pieces are aligning:
- Robotic catheter platforms are becoming more capable and clinically realistic.
- Network engineering (redundancy, monitoring, quality-of-service) is now treated as a patient-safety requirement, not an IT convenience.
- AI-assisted robotics is moving from “nice visualization feature” to “operational necessity” for consistency and scale.
In the broader “Artificial Intelligence & Robotics: Transforming Industries Worldwide” story, healthcare has often lagged manufacturing and logistics due to regulation and risk. Stroke robotics flips that narrative: the clinical stakes are so high that the incentive to adopt is unusually strong.
What remote EVT actually looks like in practice
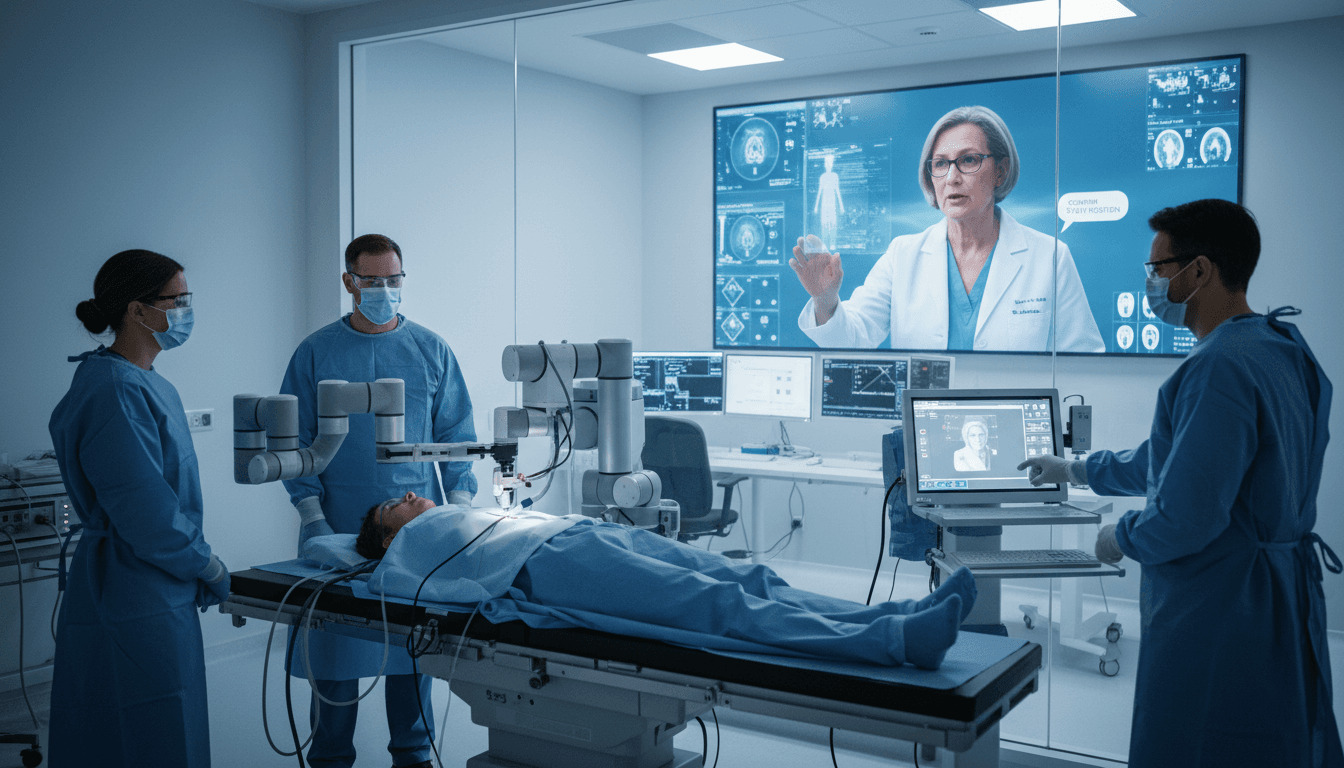
Remote EVT is a two-site procedure: a patient-side team manages the bedside setup and patient safety, while a remote specialist performs the endovascular navigation using a robotic interface.
Here’s the critical point: remote robotics doesn’t remove humans from the loop—it changes who does what.
The procedure workflow (simplified)
A realistic remote thrombectomy workflow includes:
- Patient arrival and imaging at the local hospital (CT/CTA, stroke protocol).
- Bedside preparation: sterile field, vascular access, device loading, anticoagulation and monitoring.
- Robotic control session: a remote neurointerventionalist logs into the system and navigates catheters under live fluoroscopy.
- Clot retrieval and reperfusion checks.
- Post-procedure stabilization and follow-up imaging.
The biggest misconception is that the robot “does the surgery.” In reality, the robot is a precision instrument and the network is a safety-critical bridge. The surgeon is still responsible for decisions and movements—just from a different room, city, or region.
Recent demonstrations: Toronto and transatlantic simulation
Two recent examples highlight different forms of progress:
- Toronto remote angiograms using Remedy Robotics’ N1 system showed stepwise increases in distance, including procedures between hospitals within the city. Angiography is a core component of EVT because imaging guidance is the map.
- Jacksonville (U.S.) to Dundee (Scotland) used Sentante equipment for a simulated EVT on a cadaver model with artificial blood flow—an important proof of feasibility and system behavior under real latency.
Do we need transatlantic stroke procedures? Probably not. But demonstrations at that scale prove the platform’s tolerance for real-world networking variability, and they push teams to treat resilience as non-negotiable.
Two design philosophies: AI-forward vs. “feels like the real thing”
The most useful way to compare remote surgical robots isn’t brand-to-brand. It’s philosophy-to-philosophy: how the system reduces risk and cognitive load during urgent, high-skill work.
Approach 1: AI-assisted control and smarter imaging overlays
One path (exemplified by Remedy Robotics’ direction) leans heavily into AI:
- Machine learning-assisted guidewire manipulation to smooth micro-movements and reduce unintended motion.
- Information overlays on fluoroscopy so the remote physician can interpret anatomy faster and with fewer mental jumps.
- A long-term operating model where a specialist can support multiple hospitals from a central location by “logging in” as needed.
My take: AI assistance is essential if remote EVT is going to scale beyond a handful of hero sites. If every remote case requires the same intense concentration as in-person EVT—plus additional communication overhead—you’ll hit a staffing ceiling fast.
Approach 2: Naturalistic consoles with force feedback
Another path (seen in Sentante’s system) prioritizes surgeon familiarity:
- A control console designed to match how interventionists already manipulate catheters and guidewires.
- Force feedback to mimic tactile resistance.
- Reported latency around 120 milliseconds in the transatlantic simulation—enough to notice, but not necessarily enough to prevent controlled endovascular movements.
This matters because EVT is urgent, but it isn’t like twitch gaming. Many motions are deliberate, incremental, and guided by imaging. The real goal is predictable control—and tactile cues can reduce errors when visibility is limited.
A practical stance: the winner probably combines both
Expect convergence:
- Naturalistic control to speed adoption and training
- AI assistance for stability, guidance, and standardization
- Better imaging layers that reduce cognitive load
- Built-in network monitoring to prevent unsafe movements during degraded connectivity
A good telerobotic system doesn’t just “work.” It degrades safely.
The hard part isn’t the robot—it’s the system around it
Remote robotic stroke treatment will succeed or fail based on workflow engineering, not marketing.
Latency and network resilience are patient-safety features
Remote procedures introduce latency and connection risk. The right question isn’t “Can it run over 5G?” It’s:
- What happens when bandwidth drops mid-navigation?
- What redundancy exists (dual ISP, failover, local control)?
- Does the robot detect poor connection quality and prevent harmful motion?
Systems like Remedy’s have emphasized connection-quality monitoring and safe behavior during degradation. That’s exactly the direction this needs to go.
You still need bedside clinicians—and they need a plan
Remote EVT shifts some work to the bedside team. Depending on platform design, bedside staff may handle:
- Patient communication and sedation/anesthesia coordination
- Sterility and equipment prep
- Device loading and step transitions
- Repositioning imaging equipment
- Emergency conversion plans if remote control is interrupted
If you’re evaluating telerobotics for stroke, assess the bedside burden honestly. The fastest way to fail is to assume rural hospitals can magically absorb new responsibilities without staffing, training, and protocol design.
Credentialing, liability, and reimbursement aren’t footnotes
By 2026, the technical feasibility will be less controversial than the operational governance:
- Credentialing across sites (who has privileges where?)
- Medico-legal accountability (who is responsible for each step?)
- Reimbursement models (how does payment work when expertise is remote?)
- Data governance for imaging streams, video, and robotic telemetry
These aren’t reasons to wait. They’re reasons to start building the program playbook now.
What healthcare leaders should do in 2026: a pragmatic roadmap
If you’re a health system leader, medtech partner, or policymaker trying to turn remote robotic stroke treatment into a real service, focus on measurable readiness—not hype.
1) Start with “local robotics,” then expand to remote
Many platforms will likely see earlier approvals for on-premise endovascular procedures (surgeon in the next room) before broad remote EVT. That’s not a compromise; it’s a staged safety approach.
Use local robotic cases to:
- Train teams on setup and troubleshooting
- Standardize device loading and imaging workflows
- Collect baseline procedure time data
- Build clinician trust in the interface
2) Define your “door-to-robot” metrics
Remote EVT should be evaluated with the same seriousness as stroke quality measures. Track:
- Door-to-imaging time
- Imaging-to-decision time
- Decision-to-vascular-access time
- Vascular-access-to-reperfusion time
- Connection stability incidents (with severity grading)
If remote robotics doesn’t cut total time meaningfully, it’s not meeting the core promise.
3) Build redundancy like aviation, not consumer IT
You’re not streaming a meeting. You’re steering a catheter in the brain.
Minimum expectations for a pilot program:
- Redundant network paths
- Continuous connection-quality scoring
- Clear “pause and park” behavior for the robot
- A bedside protocol for rapid takeover or stabilization
4) Treat AI as a safety layer, not a marketing bullet
AI can reduce error and cognitive load, but it must be designed with explicit guardrails:
- Movement constraints near fragile anatomy
- Automated alerts for drift, unexpected resistance patterns, or imaging inconsistencies
- Audit logs for every action and system state
A simple rule: if the AI can’t be explained to the clinical team during training, it isn’t ready for clinical reliance.
5) Choose the right first sites
Remote robotic stroke treatment should begin where it can be safely supported:
- A rural hospital with strong emergency capability and imaging
- A hub center with 24/7 neurointerventional coverage
- Shared governance and rapid escalation pathways
This isn’t about being first. It’s about being repeatable.
Where this is heading: distributed expertise as a service
Remote stroke robotics is part of a broader industrial shift: AI-powered robotics is turning scarce expertise into a networked resource. Manufacturing did it with remote monitoring and automated quality control. Logistics did it with centralized routing and autonomous fleets. Healthcare is next, but the tolerance for failure is lower—so the engineering discipline has to be higher.
Over the next few years, expect:
- Robots that support more endovascular indications (not just stroke)
- More automation in setup and device exchange to reduce bedside workload
- Standardized “remote intervention suites” in regional hospitals
- Specialist teams operating like an air-traffic-control model for urgent cases
If you’re building strategy in AI and robotics, this is the type of deployment that creates durable advantage: it improves outcomes, expands access, and can reduce the hidden costs of disability and long transfers.
The question worth asking now isn’t whether remote robotic stroke treatment will exist. It’s which health systems will turn it into reliable, everyday infrastructure—and how quickly they’ll share that capability with the communities that need it most.