Climate doulas are reshaping pregnancy care for a hotter, riskier world — blending birth support with disaster planning, heat safety, and real climate resilience.
Most people planning a pregnancy think about car seats, prenatal vitamins, and birth plans. Far fewer are mapping evacuation routes for hurricanes or figuring out how to keep a newborn cool during a week-long blackout.
Yet that’s exactly what more families in places like Florida, Texas, and Oregon are now dealing with. Climate hazards aren’t some distant future risk — they’re colliding with pregnancy and birth right now. And a new kind of support person is quietly emerging to fill the gap: the climate doula.
Here’s the thing about climate and maternal health: the science is already clear that heat waves, wildfire smoke, flooding, and storms are harming pregnancies. What’s been missing is a practical, person-to-person support system that helps pregnant people actually navigate those risks. That’s where climate-informed doulas come in.
This matters because if you care about healthy pregnancies, racial equity, or resilient communities, you can’t ignore climate anymore. The reality? It’s simpler than you think to build climate resilience into perinatal care — and the doula model might be one of the most effective ways to do it.
What is a climate doula — and why now?
A climate doula is a birth worker who integrates climate risk awareness and disaster preparedness into traditional doula care.
They still do everything a typical doula does — emotional support, advocacy, comfort measures, birth education — but with another layer: helping clients understand and prepare for climate-related threats that could affect pregnancy, birth, and postpartum.
Why now?
- Over the last decade, research has linked extreme heat and air pollution to higher rates of preterm birth, low birth weight, stillbirth, and preeclampsia.
- Climate-related disasters — from hurricanes to wildfires — are associated with increased postpartum depression and anxiety.
- Black, Indigenous, and low-income communities face both higher climate exposure and higher maternal mortality rates. That’s not an accident; it’s structural.
So the question isn’t whether climate affects pregnancy. It’s how quickly we build systems that protect the people most at risk.
Inside Florida’s climate doula pilot
Florida is quietly becoming a testbed for climate-informed maternal care.
In Miami-Dade and Broward counties, a pilot program called Doula C-Hot (short for climate and heat outreach and training) is training doulas to:
- Assess their clients’ climate risks
- Create personalized disaster and heat plans
- Connect families to climate adaptation resources
The program was co-created by doula and educator Esther Louis and physician Dr. Cheryl Holder, cofounder of Florida Clinicians for Climate Action.
How the training works
Doulas in the program are trained to have structured climate conversations with clients. They use an assessment tool that goes far beyond “Do you have AC?” and digs into real-life vulnerability, such as:
- Do you have an air conditioner and can you afford to run it?
- If the power goes out, where could you safely go?
- Can you borrow $50 in an emergency, and from whom?
- Are you in a flood zone or storm surge area?
Based on the answers, climate doulas help clients:
- Find cooling centers or clean-air shelters
- Apply for or access portable AC units or fans
- Develop an evacuation plan that accounts for late pregnancy or a newborn
- Prepare birth plans that anticipate hospital disruptions or road closures
It’s not theoretical. These doulas have already supported more than 40 clients through this model, often in neighborhoods that are hotter, more flood-prone, and less resourced.
“Where else should we start, other than with pregnant folks? That’s two lives, the next generation.” — Dr. Cheryl Holder
I agree with that framing. If a healthcare system can’t protect pregnant people and babies in a changing climate, it’s failing at the most basic level.
How climate change harms pregnancy — in plain language
You don’t need a medical degree to understand the problem. The mechanisms are pretty straightforward.
Extreme heat
High temperatures are one of the most well-documented climate threats to pregnancy.
Heat exposure is linked to:
- Preterm birth: Studies have shown higher risk of early delivery during heat waves.
- Low birth weight and stillbirth: Chronic exposure to high temperatures can stress both the pregnant body and the placenta.
- Preeclampsia and hypertension: Heat can worsen cardiovascular strain, which is already elevated in pregnancy.
Add in the reality that many pregnant people work outdoors, have jobs without paid leave, or can’t afford round-the-clock cooling, and the risk multiplies.
Air pollution and wildfire smoke
Fine particulate matter from traffic, industry, and especially wildfires penetrates deep into the lungs and bloodstream. For pregnant people, that can mean:
- Increased risk of preterm birth
- Higher odds of low birth weight
- Greater chance of hypertensive disorders
Babies exposed in utero to heavy smoke or pollution are more likely to have respiratory and developmental challenges later.
Disasters, displacement, and mental health
Storms, floods, and long-term displacement don’t just disrupt access to clinics. They also spike stress hormones and can derail support systems.
Researchers are finding higher rates of:
- Postpartum depression and anxiety after climate-related disasters
- Traumatic birth experiences when care is rushed, interrupted, or relocated
Climate doulas are stepping into that vacuum — not to replace clinical care, but to make sure families don’t face those events alone or unprepared.
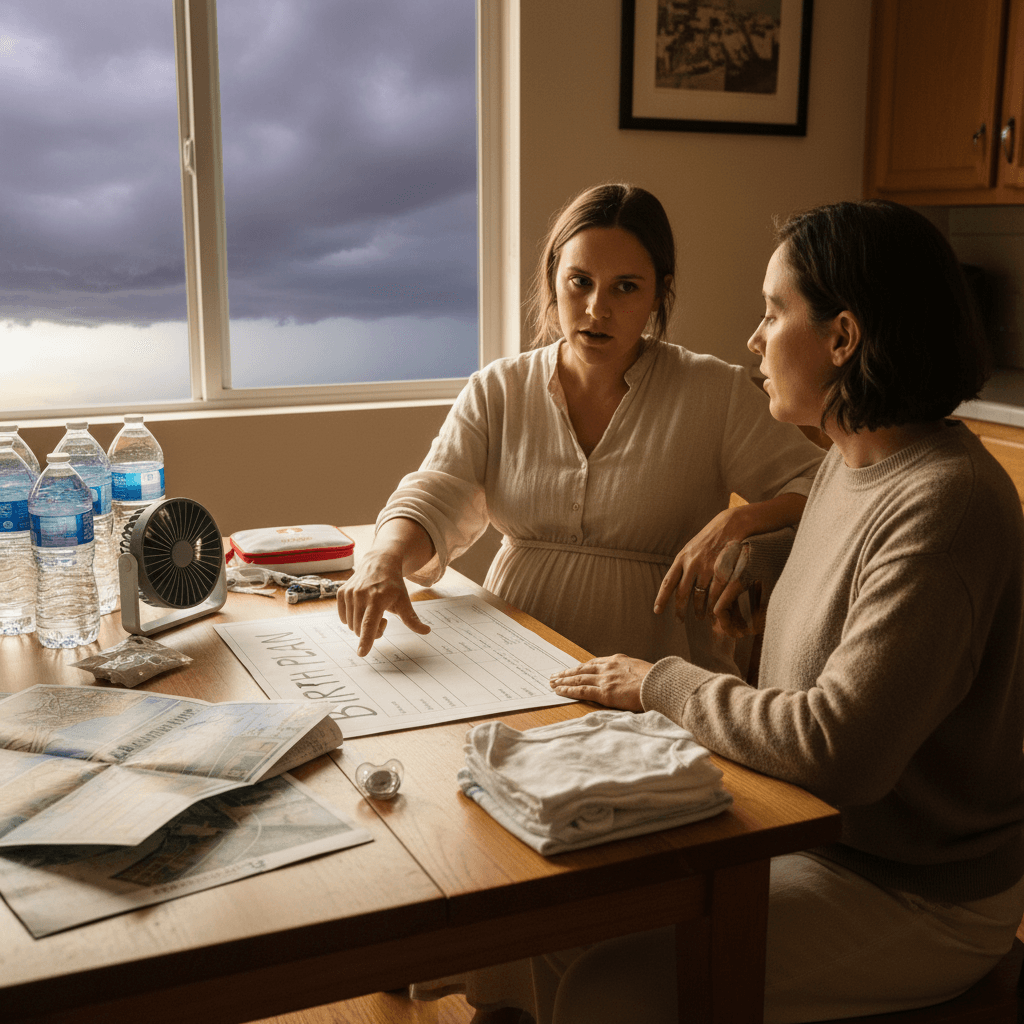
What climate doulas actually do with families
It’s easy to talk about “resilience” in abstract terms. Climate doulas make it concrete.
Here’s what this looks like in practice.
1. Hazard mapping and personal risk assessment
Climate doulas help clients answer questions like:
- What are the top threats in this region? (Heat waves, hurricanes, wildfires, ice storms?)
- How pregnant will I be during the peak risk season?
- Is my housing structurally safe in a flood, storm, or heat emergency?
- Do I rely on medical equipment (like insulin refrigeration) that needs power?
This turns climate from a vague worry into a specific, manageable scenario.
2. Disaster and evacuation planning for pregnancy
Standard emergency plans rarely account for someone who is 38 weeks pregnant or has a 2-week-old baby.
Climate doulas help families:
- Decide when they’d leave before a major storm, and who drives
- Identify backup hospitals or birth centers if the closest one is compromised
- Pack a climate-aware go bag, including:
- Copies of prenatal records
- Medications and prenatal vitamins
- Cooling tools (hand fans, cooling towels, electrolyte packets)
- Formula and safe-feeding tools if needed
In some cases, doulas even caravan with clients during evacuations, providing emotional support and on-the-road problem-solving.
3. Heat and air quality strategies
For heat and smoke, climate doulas focus on practical, low-tech steps as well as system-level resources.
For heat:
- Set thresholds: “If the heat index goes above X and your home is above Y at night, here’s the plan.”
- Teach cooling strategies that don’t depend solely on AC — cool baths, wet sheets, shaded rest, hydration routines.
- Help clients enroll in utility assistance or find cooling centers.
For smoke and air pollution:
- Show families how to check air quality levels and what different colors mean for pregnancy.
- Create one “clean room” at home using a HEPA filter or DIY filter fan.
- Adjust outdoor appointments, exercise, or work schedules when smoke is heavy.
4. Safe infant feeding in emergencies
Doulas in places like Houston and New Orleans are already guiding parents through questions like:
- How long is breast milk safe in a fridge during a power outage?
- How can you sterilize bottles if you don’t have electricity or clean running water?
- How do you find privacy and safety to breastfeed in a crowded shelter?
These aren’t fringe scenarios anymore. They’re becoming seasonal realities.
Barriers — and why policy has to catch up
Here’s the uncomfortable part: the families who need climate doulas the most are often the least able to pay for them.
A few key tensions:
- Cost of doula care: Full-spectrum doula services can run into the thousands of dollars per pregnancy.
- Medicaid coverage is patchy: Some states now reimburse doulas under Medicaid, but the process is often narrow and bureaucratic. Community-based doulas — especially those trained outside mainstream certifying bodies — are frequently excluded.
- Medicaid itself is under political attack in multiple states, despite covering around 4 in 10 births nationally.
That’s why I think any serious climate-resilient health strategy has to include:
- Expanded Medicaid coverage for doulas, with flexibility to recognize community-rooted training
- Funding for climate-specific doula training, especially for Black, Indigenous, and immigrant doulas
- Support for language access, so materials exist in Spanish, Haitian Creole, and other community languages — not just English
If we keep climate doula care as a boutique service for those who can pay out of pocket, we’ll simply widen the gap in maternal outcomes.
How providers and communities can act now
You don’t need to wait for a formal program to bring climate support into pregnancy care. There’s a better way to approach this: start small, start local, and center the people already doing the work.
For doulas and birth workers
- Integrate three climate questions into your standard intake: housing safety, heat access, and evacuation support.
- Build a simple local resource list: cooling centers, disaster hotlines, mutual aid groups, clinics that accept Medicaid.
- Partner with clinicians or public health groups interested in climate — they often have data and materials, but lack trusted community messengers.
For clinicians and hospitals
- Refer high-risk patients (especially in late pregnancy during peak climate seasons) to climate-informed doulas or community health workers.
- Add climate risk screening to prenatal visits: “Will you be in your third trimester during wildfire season / hurricane season / peak heat?”
- Advocate internally to cover doula services in hospital community benefit or social determinants of health budgets.
For policymakers and funders
- Treat climate maternal health as infrastructure, not charity.
- Fund train-the-trainer programs like the ones emerging in Florida and Oregon.
- Require Medicaid doula reimbursement rules that don’t exclude community-based training.
If you’re pregnant now: simple steps to build climate resilience
If you’re currently pregnant or planning to be, especially in a climate-vulnerable area, here are a few practical moves you can make this week:
- Map your risks: Identify your top two local climate threats (heat, wildfire, flooding, hurricanes, ice storms) and when they’re most likely.
- Ask your doula or provider directly: “How should I prepare for [heat waves / hurricanes / smoke] during my third trimester?” If they don’t have answers yet, that’s a cue — not a dead end.
- Create a pregnancy-specific go bag: Include medical records, medications, a list of emergency contacts, and basic cooling or air quality tools.
- Find your safe places: Know where you’d go if your home became unsafe — friend’s house, relative, community center, shelter — before you need it.
None of this removes the responsibility from governments or health systems. But it does give you more control in a situation that often feels overwhelming.
Where this is heading
Climate doulas are still new, but they’re not a fringe idea. They’re an early glimpse of what health care will look like as the climate crisis intensifies: more relational, more preventative, and far more honest about environmental reality.
Pregnancy will always involve uncertainty. Climate change adds another layer — but it doesn’t need to be paralyzing. With the right support, families can plan, adapt, and protect both parent and baby.
The real question for the next few years is simple: will climate-informed support like this stay scattered and underfunded, or will we treat it as essential care?
If you work in health, birth, policy, or community organizing, now is the time to decide which side of that line you’re on.