Remote stroke robotics can cut hours off treatment time for rural patients. See how AI-assisted telerobotics is reshaping EVT access and outcomes.
Remote Stroke Robotics: Faster Care for Rural Patients
A large-vessel stroke doesn’t wait for the nearest specialist to finish rounds—or for a helicopter to land. The brutal math is well known in neurology: about 2 million neurons die every minute that blood flow is blocked. Over an hour, that’s roughly 3.6 years of typical age-related brain cell loss. When you hear clinicians say “time is brain,” they’re not being dramatic.
Here’s the part most healthcare systems still get wrong: we’ve built world-class stroke capability, then concentrated it in a small number of urban hospitals. For patients in remote regions—Darwin in northern Australia is a vivid example—getting to an endovascular thrombectomy (EVT) center can take six hours or more, plus an expensive aeromedical transfer. That delay isn’t just inconvenient; it’s the difference between returning to work and needing long-term care.
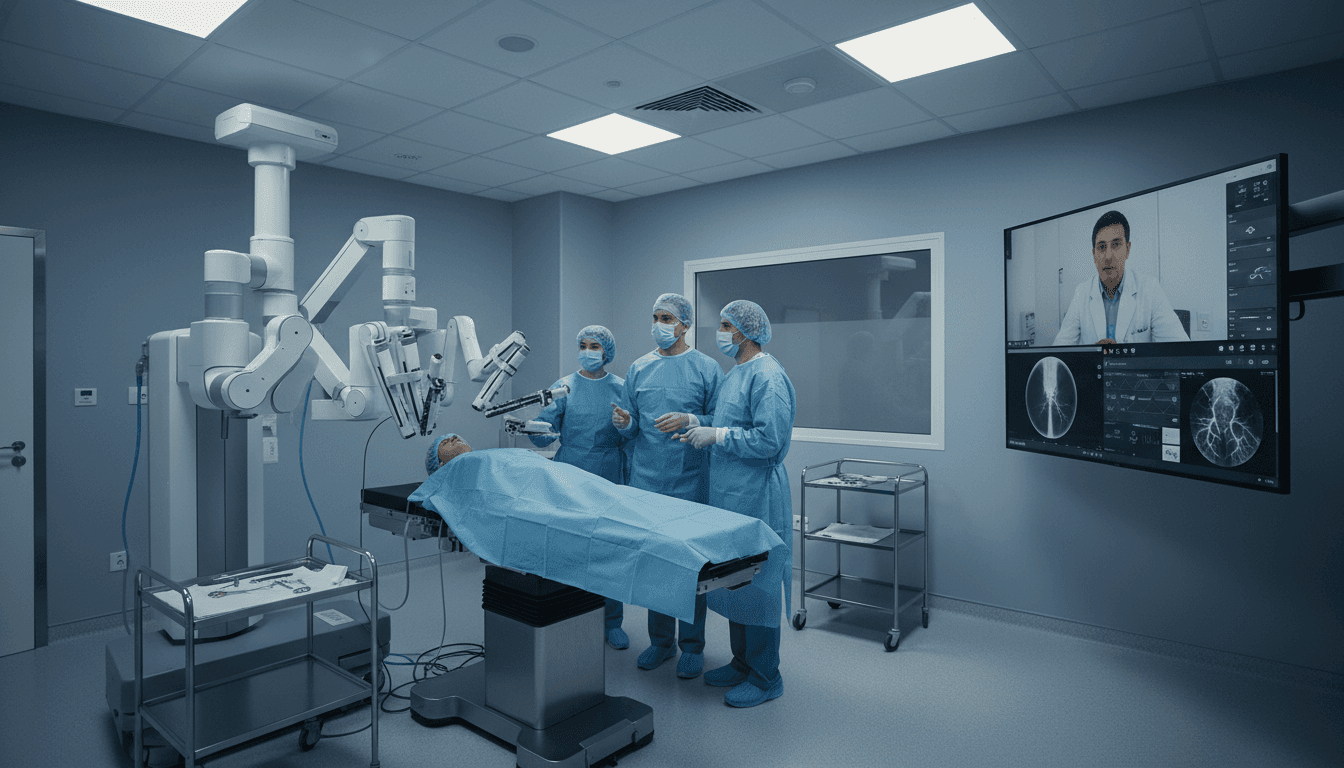
Remote robotics is starting to offer a practical fix. Recent demonstrations—robot-assisted angiograms performed remotely in Toronto using Remedy Robotics’ N1 system, and a simulated transatlantic EVT using Sentante equipment—show that telerobotic neurointervention is moving from “nice demo” to “deployment planning.” In the broader Artificial Intelligence & Robotics: Transforming Industries Worldwide series, this is one of the clearest examples of AI and robotics doing what they do best: bringing scarce expertise to where demand is, not where the experts live.
Why remote robotic stroke treatment matters (beyond the headline)
Remote robotic EVT matters because it attacks the largest driver of stroke outcomes: time-to-treatment. Hospitals can’t recruit neurointerventionalists everywhere. Training takes years, and many regions simply don’t have the case volume or funding to support a full-time team.
The current workaround is transport: take the patient to the expert. But for a time-critical condition, transport is a tax on outcomes.
A useful way to say it: in rural stroke care, geography is a clinical risk factor.
Remote surgical robotics flips that equation. Put a robotic platform in a regional hospital, connect it to a specialist in a metro center, and you potentially:
- Save hours by avoiding transfers
- Increase EVT eligibility by keeping patients inside the treatment window
- Reduce long-term disability, which is where the lifetime cost of stroke often sits
- Expand coverage without forcing every community to staff a full specialist team
This is also a real “industry transformation” moment. The hospital isn’t just a building with departments anymore—it becomes a node on a clinical network, with robotics acting as the physical interface.
What’s actually being done remotely—and what’s not (yet)
The near-term reality is hybrid care: remote control for the delicate intravascular work, local staff for bedside tasks. EVT is not a simple procedure you can run from a laptop with no onsite support.
EVT in plain language
Endovascular thrombectomy treats strokes caused by large clots blocking blood flow to the brain. A clinician navigates catheters and guidewires through blood vessels (often entering via the femoral artery in the groin) to reach the blockage and remove it. Imaging—typically X-ray fluoroscopy—guides the journey.
When robotics enters the picture, the robot doesn’t “decide to treat stroke.” It becomes a highly controlled instrument that:
- Moves catheters/guidewires with precision
- Reduces operator strain and variability
- Enables remote operation when connected to a secure, high-quality network
What recent demonstrations tell us
The Toronto work showed a progression of remote neurovascular imaging (angiograms) using Remedy Robotics’ N1 system, ultimately between crosstown hospitals. The transatlantic simulation—a surgeon in Jacksonville controlling equipment in Dundee—used Sentante’s system on a cadaver model with artificial blood flow.
A transatlantic case isn’t the typical clinical need; it’s a stress test. The important point is simpler: remote operation is technically feasible, and the remaining work is about clinical validation, workflow design, and regulation.
Two design philosophies: AI-first vs “feels like your hands”
Remote robotics in healthcare is splitting into two strong approaches, and both are rational. One leans into AI assistance and software overlays; the other prioritizes familiar tactile control with force feedback.
Remedy Robotics: AI-assisted control and image overlays
Remedy’s stated direction emphasizes artificial intelligence and software mediation—machine learning that helps with guidewire manipulation and adds informational overlays on top of X-ray imaging. The long-term operational vision is compelling for health systems: a specialist could log into a platform and support multiple hospitals as demand spikes.
From an “AI and robotics transforming industries” lens, that’s a classic scaling model:
- Centralize scarce talent
- Distribute robotic “execution” endpoints
- Use AI to reduce cognitive load and standardize steps
It’s not about replacing the specialist. It’s about making one specialist cover more ground safely.
Sentante: intuitive controls and force feedback
Sentante’s approach focuses on replicating the feel of manual EVT, including force feedback that mimics resistance a surgeon would sense in person. In its demonstration, reported latency was around 120 milliseconds, and clinicians described the experience as naturalistic.
I’m opinionated here: in high-stakes procedures, intuition is a safety feature. If a system maps cleanly to what clinicians already know, adoption gets easier, training curves shorten, and errors become less likely.
Sentante hasn’t yet implemented AI-assisted movements, but it plans to capture extensive training data from images and force measurements—an approach that often precedes reliable clinical AI.
The hard problems: network reliability, bedside staffing, and liability
The biggest barriers to remote stroke robotics aren’t “can the robot move?” They’re operational realities: connectivity, staffing, and governance.
Connectivity and latency: “fast enough” beats “perfect”
EVT is urgent, but it’s not a reflex-based activity like competitive gaming. Small delays can be manageable—until they aren’t. What matters more than raw latency is predictability.
Remote robotic intervention needs:
- Low, stable latency (jitter is often worse than delay)
- Redundant connections so a single drop doesn’t force an abort
- Safety states so the robot doesn’t make harmful movements if signal quality degrades
One detail that should reassure hospital buyers: some systems are being designed to actively monitor connection quality and refuse unsafe actions when the link is compromised.
The bedside team doesn’t disappear
Remote doesn’t mean “no humans onsite.” It means the most specialized hands can be remote while local clinicians handle:
- Patient prep, consent processes, and monitoring
- Sterile setup and instrument loading
- Imaging repositioning
- Emergency contingency actions if needed
As one interventional radiologist noted in the source, robotics still depends on bedside interventionists. The winning deployments will treat bedside staff as first-class users—not as an afterthought.
Liability and clinical governance need to be designed in, not bolted on
If you’re a health system leader, ask early:
- Who is the operating physician of record—the remote specialist, the onsite clinician, or both?
- What are the escalation steps if imaging quality drops or anatomy is difficult?
- How is the procedure documented (video, logs, robot telemetry)?
- What’s the credentialing model across facilities?
Remote robotic surgery will scale only when the governance model is as mature as the technology.
The path to clinical use in 2026 and beyond
The fastest route to routine remote EVT is likely stepwise: local robotic procedures first, then remote expansion. That pattern is common in regulated industries. Systems prove reliability and safety in a controlled environment, then add complexity.
Remedy has a 2026 clinical trial planned for on-premise neurointerventions, and it’s partnered with the Australian Stroke Alliance toward a future trial for remote procedures. Sentante is aiming for EU market entry for peripheral vascular interventions and holds a U.S. FDA breakthrough device designation for remote stroke treatment.
This staging also solves a practical issue: keeping teams practiced. If a robot can be used for a broader set of endovascular procedures—peripheral vascular interventions, for example—local teams stay familiar with setup and troubleshooting. That matters when the “big case” arrives at 2 a.m.
A point that often gets missed: if a platform can eventually support 30+ conditions, the business case strengthens dramatically. The robot isn’t “a stroke machine.” It becomes infrastructure, like imaging or anesthesia systems.
What hospital leaders should do now (if you want access and outcomes)
The actionable move is to prepare your stroke network for robotics—before you buy a robot. Technology adoption fails more from workflow mismatch than from hardware quality.
Here’s a practical checklist I’d use if I were advising a regional health network.
1) Map your “time-to-treatment” bottlenecks
Quantify:
- Door-to-CT time
- Door-to-CTA (angiography) time
- Door-to-needle (thrombolysis) time
- Door-in-door-out times for transfers
- Average transfer time to EVT centers
Robotics only helps if it removes your biggest delays.
2) Build a tiered staffing model
Plan for:
- A small onsite team trained in sterile setup, imaging, and contingency actions
- A remote specialist roster with defined on-call expectations
- Simulation training blocks (quarterly is a good starting target)
3) Invest in network resilience like it’s clinical equipment
Treat connectivity as part of the device ecosystem:
- Redundant internet pathways
- Dedicated bandwidth and quality-of-service policies
- Continuous monitoring and incident response
If you wouldn’t accept an unreliable ventilator, don’t accept an unreliable network.
4) Choose KPIs that reflect patient outcomes, not just utilization
Measure:
- Functional outcomes (e.g., discharge disposition, rehab intensity)
- Complication rates
- Time saved versus transfer model
- Percentage of eligible patients receiving EVT
Robotics should earn its keep by improving outcomes and access—period.
People also ask: quick answers for decision-makers
Can remote robotic surgery treat strokes today?
Not routinely. The field is transitioning from demonstrations and simulations toward clinical trials and staged approvals, with local robotic interventions often preceding remote EVT.
Is latency a deal-breaker?
No—unstable latency is the bigger risk. EVT can tolerate some delay, but remote systems need predictable performance, redundancy, and safe fallback behavior.
Will AI replace neurointerventionalists?
No. The most realistic near-term impact is AI-assisted precision and standardization, enabling specialists to support more patients across a wider geography.
Where this fits in the bigger AI & robotics story
Remote EVT robotics is a strong case study for the broader theme of this series: AI and robotics shift “where work happens.” In factories, robots move production closer to demand. In healthcare, robots move expertise closer to patients.
Rural healthcare inequality isn’t solved by one invention, but remote robotic stroke treatment is one of the few approaches that directly targets the core constraint: specialist scarcity combined with travel time. If the next two years bring solid clinical trial results and clear credentialing models, regional hospitals could stop treating “transfer” as the default stroke plan.
The forward-looking question worth sitting with is this: When robotics turns hospitals into connected networks, which other time-critical services should be next—cardiac cath, trauma, neonatal care? If you’re building a healthcare strategy for 2026, that’s not a futuristic thought experiment. It’s a roadmap decision.